Silicon nitride is an ideal material for medical implants. Its wear rate is extremely low, and the wear particles are soluble and can be cleared from the body. Silicon nitride is chemically resistant, and it has a high dielectric constant, which confers resistance to fretting corrosion.
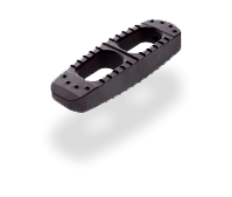
When used to make spinal fusion implants, silicon nitride has the flexibility of a dense, porous, or combined architecture that can mimic the cortical-cancellous structure of bone1, 2. Cumulative silicon nitride implantations through 2018 total about 35,000. Of these, fewer than 30 FDA-reportable adverse events manifested, with no implant-related infections relative to an industry standard of 3–10%